Benefits packages today are like a prix fixe menu. What if they were more like a buffet?
From tuition reimbursement to in vitro fertilization, the variety of benefits that employers can offer to workers has never been more vast. On paper, employees should have more choice regarding their benefits than ever.
But in practice, this is rarely the case.
Crafting a “one-size-fits-all” benefits package that satisfies the diverse needs of Gen Z, remote employees, and working parents without overspending has proven difficult for HR departments to nail down. On top of this, the customization options within each benefit are often nonexistent, resulting in a frustrating experience for workers that doesn’t promote optimal benefits usage.
With companies shifting their priority from recruiting to retention in 2023, HR departments need a solution that results in a satisfactory benefits experience for all employees[1]. Luckily, that solution has a name, and it’s called “a la carte” benefits.
In this report, with help from a survey of nearly 300 benefits leaders*, we’ll go over the problems with traditional benefits packages, how a la carte benefits can fix them, and best practices for implementing this benefits solution with help from the right software at your organization.
/ Key findings
Your benefits package is critical to employee retention: A majority of benefits leaders (57%) say employee benefits are extremely important to retaining top talent. Among large businesses (1,001+ employees), that number jumps to 67%.
Employees have to make too many benefits decisions: 62% of benefits leaders agree that the amount of decisions employees have to make about their benefits is overwhelming.
Some employees lack proper decision support from HR: Close to 1 in 5 benefits leaders (19%) say they offer little to no decision support to employees during open enrollment.
3 problems with traditional benefits packages
Not only do a majority of surveyed benefits leaders (57%) say employee benefits are extremely important to retaining top talent, but Gartner adds that when employees find benefits relevant to their needs, their performance improves by 12%[2].
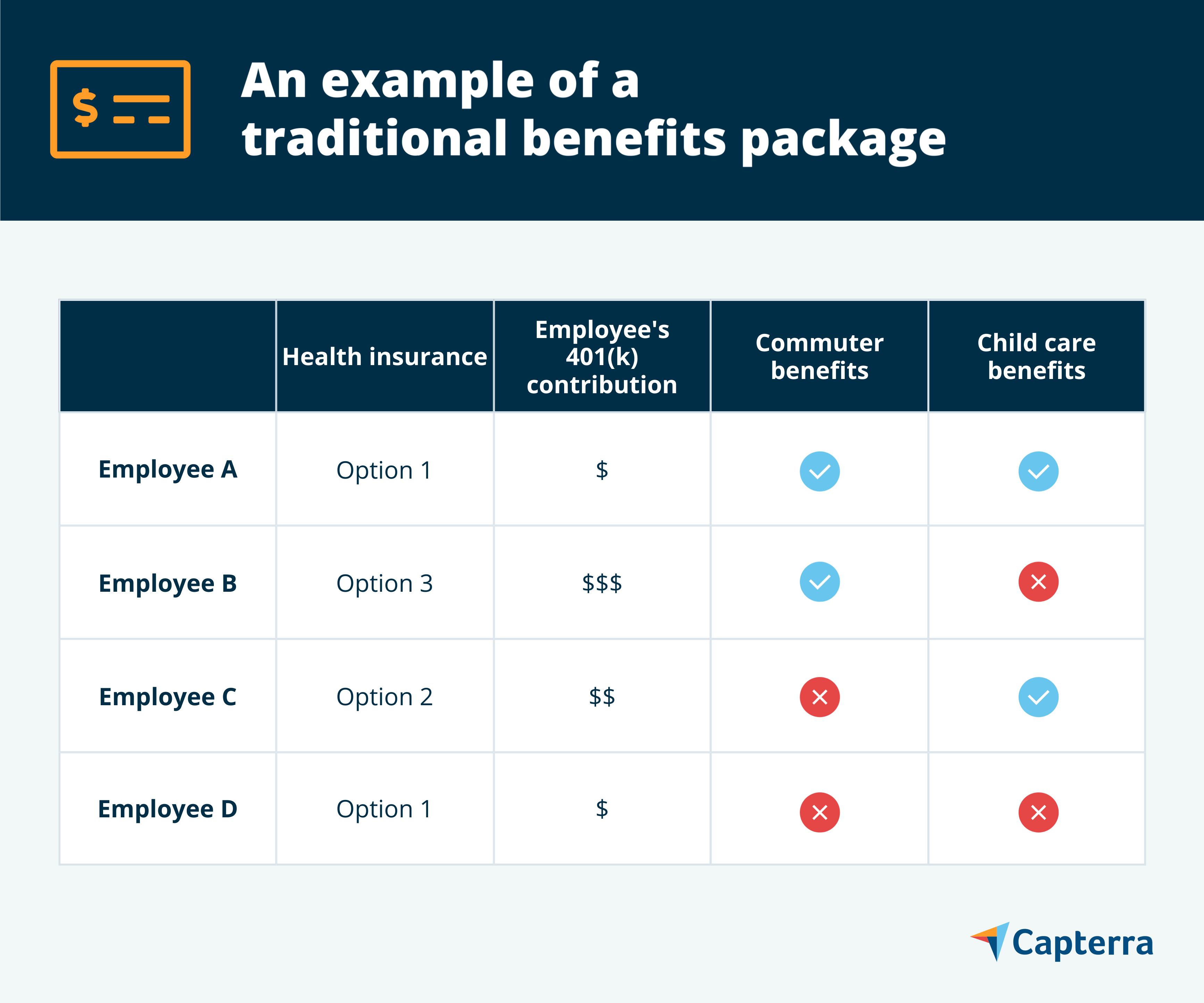
Offering a benefits package that employees can finetune is important. But if you look at a traditional benefits package—like in the example below—the amount of choice employees have with their benefits varies widely.
On the one hand, workers can decide exactly how much money they contribute to their 401(k) or select from a handful of different health insurance plans. But for more fringe benefits, such as child care, the only option employees often have is to opt in or opt out of a set amount of coverage.
At a time when consumers expect more personalization of their experiences than ever, traditional benefits packages fail to deliver. Here are three reasons why:
1. Employers have to limit how many benefits they offer to keep costs down
Without limits on how many benefits employees can sign up for, any time a company adds a new benefit to their package—even a voluntary benefit where employees have to pay into it through payroll deductions—it also adds cost.
If a company starts offering tuition reimbursement, for example, interested employees won’t stop enrolling in dental insurance. They’ll simply add it on to the benefits they already have.
And with benefits costs on the rise (they increased nearly five percent, on average, over the course of 2022), employers are incentivized to prioritize the benefits that will be used the most and provide the highest ROI, which ends up limiting the benefits available to employees[3].
2. Employees can’t customize how much of a benefit they receive
Just because two employees are enrolled in a specific benefit doesn’t mean they assign it the same value.
In the example above, Employees A and B are both enrolled in commuter benefits. While Employee A only comes into the office twice per week, however, Employee B comes in every day—from far outside city limits, and on public transit.
Employee B would love to have more commuter benefits than Employee A, but they end up getting the same amount of coverage. This frustrating imbalance happens with a lot of benefits.
3. Traditional packages punish non-users
Ideally, employees who don’t find any of your benefits relevant to their needs would instead receive additional compensation in a one-to-one ratio. In some cases, employees may be able to successfully negotiate this approach when they accept a job offer.
But more often, employees who don’t sign up for benefits end up getting less rewards (salary + benefits) overall.
How a la carte benefits work
A la carte benefits show real promise in fixing the issues with traditional benefits packages.
With a la carte benefits, each employee is given a set amount of money (usually in the form of a “flexible benefits fund”) at open enrollment that they then distribute between different benefits options as they see fit. If they have any money leftover after distributing their fund between different benefits, they get to pocket it as additional income.
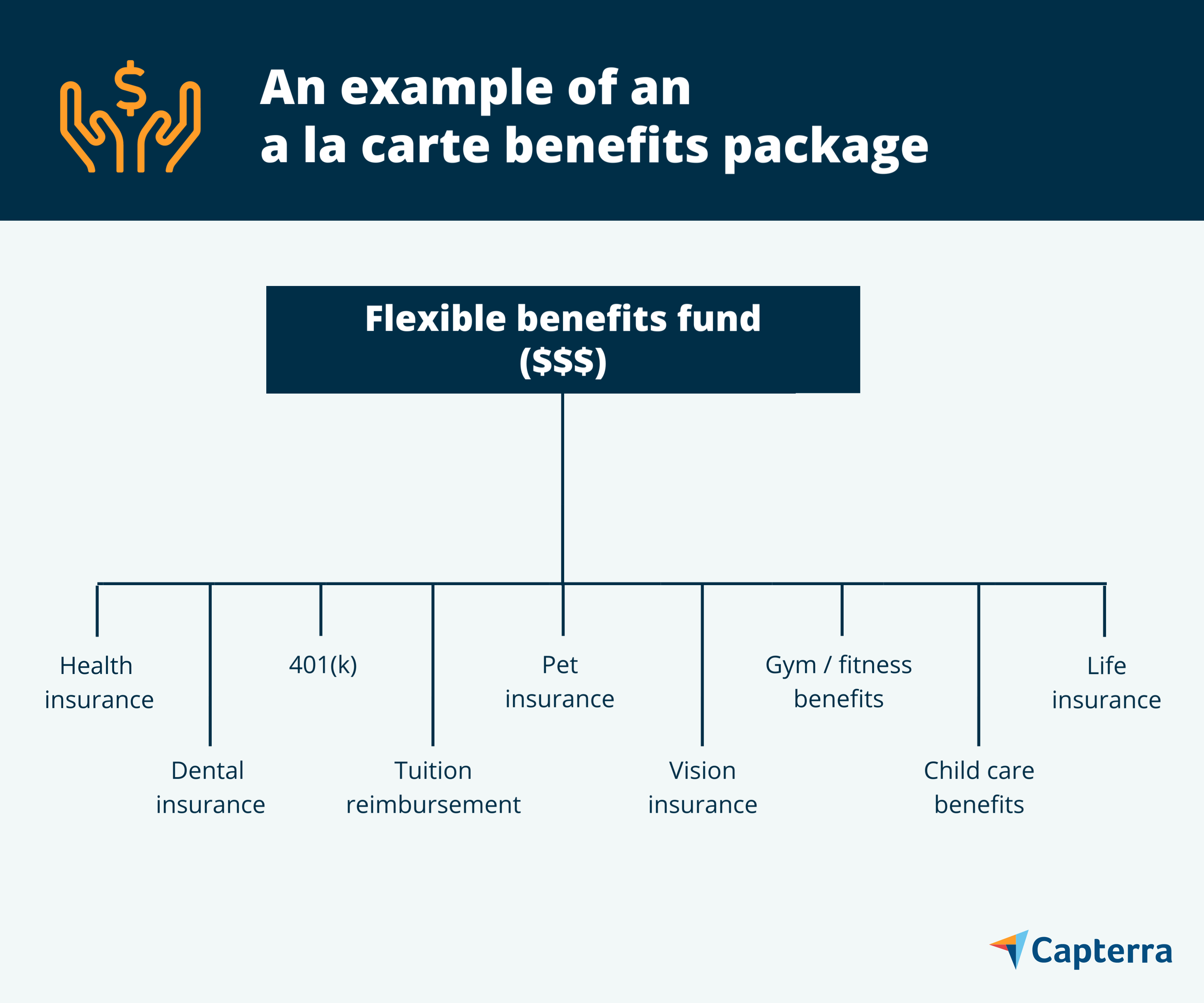
This benefits approach has a few advantages:
Because each employee gets the same amount of money to allocate (which keeps the cost of benefits per employee consistent), companies can offer more benefits without significantly raising costs.
Employees can allocate as much—or as little—to each benefit as they want (within the limit of their benefits fund).
If employees decide there aren’t many benefits relevant to their needs, they can pocket their allocation as extra income—avoiding punishment for not enrolling in benefits.
A la carte benefits are still fairly new; Gartner says only eight percent of organizations have started experimenting with them. But, when asked if they’d consider implementing a la carte benefits at their employer, 36% of HR leaders expressed interest[2].
3 ways to minimize choice paralysis with a la carte benefits
While a la carte benefits solve a lot of problems, they do carry one major downside: the number of choices employees have to make about their benefits increases significantly.
In our survey, 62% of benefits leaders say that the amount of decisions employees have to make about their benefits is overwhelming. And that’s with traditional benefits packages. With a la carte benefits, employees not only have to decide which benefits they want, but how much money to allocate to each of them.
This situation can be both stressful and lead to poor benefits decisions if implemented poorly. Here are three ways your department can improve the results of your a la carte benefits program.
1. Make important benefits mandatory, and bundle others in an LSA
Choice is great to an extent, but the last thing you want is your employees to go wild with their benefits and decide to not allocate anything to something critical, like health insurance. That’s too risky for both the employee and the organization.
Making health insurance and other important benefits mandatory with a required minimum of fund allocation reduces the amount of choices employees have to make, and helps them avoid underutilization.
Another way to help employees is by bundling your wellbeing benefits—things like gym subsidies, child care, and therapy—into what’s called a lifestyle spending account (LSA).
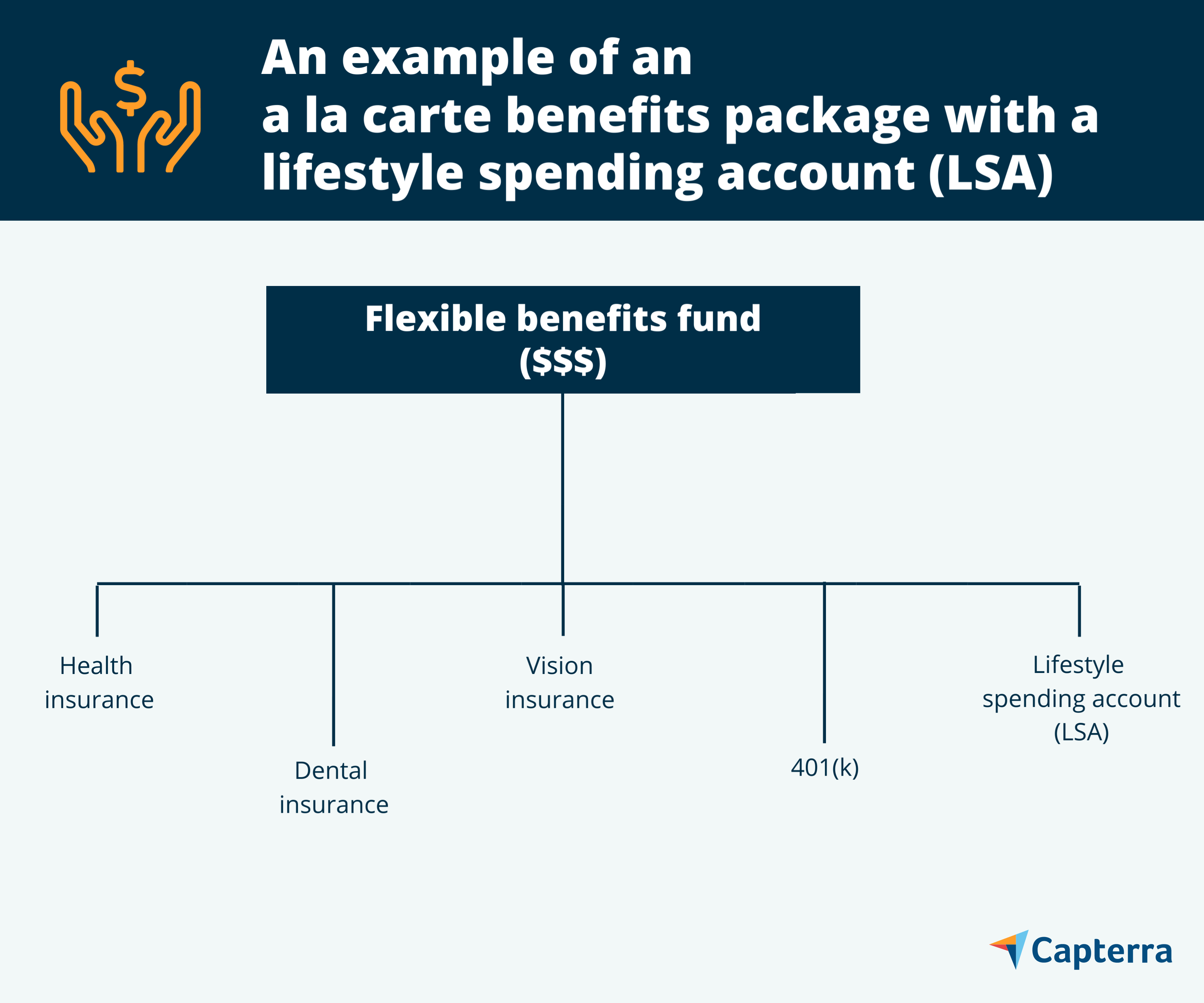
Not only do LSAs reduce the number of decisions employees have to make at open enrollment, but because LSAs don’t carry any tax benefits like a health savings account (HSA), the offerings within an LSA can run a wide gamut.
Another benefit of LSAs is that employees can use the account as needed throughout the year, instead of being forced to make decisions across multiple benefits at a single point in time.
2. Offer better decision support through software
Employees rely on HR to provide benefits information and help them make decisions. If your decision support is lacking, the a la carte benefits enrollment process will only lead to more confusion and poor benefits choices.
Unfortunately, our survey found that one percent of organizations offer no benefits decision support whatsoever, and 18% only offer simple guides that explain advantages and costs. HR departments need to do better.
The first way HR departments can upgrade their decision support is through surveys. Filling out a survey about medical needs and benefits preferences takes much less time for employees to do than pouring through benefits documentation, and is a more personalized form of support overall.
The only downside with surveys is that they rely on employees remembering all of their benefits needs and usage from the previous year, which is difficult. An even better solution is to recommend benefits to employees through their own claims data. As this approach is much less reliant on employee memory, this method helps employees make more accurate benefits decisions.
Best of all, your department doesn’t have to offer this level of personalized support the manual way. Through benefit decision support platforms, chatbots use surveys and claims data to automatically guide employees during open enrollment.
3. Personalize how benefits are communicated to employees
At the beginning, we talked about how hard it is to make a standard benefits package for a diverse range of employees. The same can be said for how benefits are communicated to those employees.
Sending regular emails reminding your entire org about the vision benefits your offer is great, but it’s not going to be relevant to every employee. Instead, HR departments should send targeted communications based on employee characteristics to increase benefits awareness and usage.
Generational segmentation is a good place to start, as younger workers will usually have different benefit needs than older workers. But why stop there? Creating personas that represent different types of employees in your organization with different benefits needs—and basing your benefits marketing around them—will result in communications that attract more attention and better inform employees.
To retain top talent, consider going a la carte with your benefits
As shockingly simple as the solution is at its core—giving employees money and letting them use it on benefits as they please—the advantages of a la carte benefits over the traditional benefits package are clear.
With a diverse workforce spread across multiple generations, locations, and stages of life, and retention becoming a top priority for HR departments big and small, companies need to give employees the benefits flexibility that the a la carte approach provides.
Keeping a close eye on flexible benefits funds and providing personalized decision support at open enrollment is critical to a la carte benefits success. If your current benefits administration platform isn’t up to the task, consider an upgrade.
Capterra's Shortlist
Our Shortlist of the best benefits administration systems out there based on real user reviews is a great place to start.
